|
 |
- Search
| Korean J Schizophr Res > Volume 26(2); 2023 > Article |
|
Abstract
Objectives
The aim of this study was to investigate whether patients with schizophrenia are aware of the current status and have accurate information about COVID-19.
Methods
The participants consisted of 161 inpatients and 117 outpatients with schizophrenia and 40 normal controls. The subjects completed self-report questionnaires measuring changes in their daily life, their perceptions of the current status of COVID-19 and their basic knowledge about the disease.
Results
Compared to the normal control group, the inpatients and outpatients with schizophrenia underestimated the cumulative number of confirmed COVID-19 cases and overestimated the mortality rate of COVID-19. The mortality rates of COVID-19 and the common cold were higher in the order of inpatients, outpatients, and normal controls. The main route of SARS-CoV-2 infection and the main symptoms of COVID-19 were accurately recognized by more than 95% in the normal group and more than 80% in outpatients, but inpatients chose the correct answers at a lower rate. In the questions about misperceptions about COVID-19, the correct answer rate was high in the order of normal controls, outpatients, and inpatients. Most patients with schizophrenia obtained information about COVID-19 on TV, while most normal controls collected information through the internet.
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). COVID-19 has spread rapidly to almost all countries around the world, with more than 600 million cases and more than 6 million deaths as of September 14, 2022 [1]. The disease has had a great impact on individual lives and global health.
In previous studies, it has been reported that patients with severe mental illness are vulnerable to infectious diseases such as COVID-19 [2,3]. The reasons include a lack of judgment [4,5], inadequate awareness of risks [6], lack of usual personal hygiene management [7], difficulty in managing underlying diseases [8,9], group housing facilities [5,10] and lower access to adequate medical services [8,9,11].
For viral respiratory diseases such as COVID-19, participation in the infection prevention rules recommended by the state plays an important role in preventing the spread of infection. To participate in these preventative measures, an accurate understanding of the disease is essential. According to a telephone survey, three-quarters of patients with severe mental illness were not aware of the symptoms and precautions of COVID-19 [12].
Among severe mental illnesses, schizophrenia, in particular, is characterized by impairment of cognition and decision-making ability [5]. Patients with schizophrenia are expected to have more difficulty understanding information about infectious diseases and carrying out preventive measures [9,13] than those with other mental illnesses. A previous study [12] reported the perception of COVID-19 in severe mental illnesses such as depressive disorders, bipolar disorder, and schizophrenia, but no study has reported the perception of COVID-19 only in patients with schizophrenia.
This study aims to investigate the perception of information and the current status of COVID-19 among patients with schizophrenia and how it affects their daily lives. Our hypothesis is that patients with schizophrenia will have a lower level of awareness of COVID-19 than normal controls, and the disease will have less impact on their daily lives. Additionally, inpatients in closed environments will not know as much about COVID-19 as outpatients.
The subjects of the study completed the questionnaire from September 8 to 29 2020. The subjects consisted of those who were either hospitalized or outpatients at Yongin Mental Hospital during the same period, and patients diagnosed with schizophrenia by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) were targeted. Among them, participants were limited to adults over the age of 19 and those who could understand and participate in the study by reading consent forms and questionnaires by themselves. To compare the patients’ perceptions about COVID-19 to those of the general public, a questionnaire was completed by and received from 40 medical and administrative staff who worked at Yongin Mental Hospital and did not have a psychiatric history. The purpose and method of the study were fully explained to all study participants, and written consent was obtained. This study was approved by the Yongin Mental Hospital Institutional Review Board (YIMH-IRB 2020-20, the date of ethics committee approval; September 2, 2020).
The research subjects were given self-report questionnaires and asked to answer questions regarding their personal information (age, gender, education). Basic knowledge, such as the current status of COVID-19 in Korea and changes made to their daily life due to COVID-19, as well as questions regarding the number of cumulative confirmed cases, the probability of death, the infection route of SARS-CoV-2, methods for preventing infection, and main symptoms of COVID-19 were confirmed through a self-report questionnaire developed by the authors. The contents of the survey were referenced in a study of the general population [14], and each question was presented simply and clearly in one sentence so that schizophrenia patients could easily understand it.
The questionnaires consisted of a total of 10 items. One item asked about changes experienced in the respondents’ daily lives. Three items presented multiple choice questions about the current status of COVID-19 (the cumulative number of confirmed cases and the mortality rate) to test the respondents’ knowledge about COVID-19, the actions to prevent infection (multiple responses), the main paths of infection, and the main symptoms (multiple responses) of the disease. One item consisting of 8 sentences was answered with yes or no. This confirmed the respondents’ misconceptions about COVID-19.
Cronbach’s alpha reliability coefficient was 0.66, which was considered satisfactory for this study.
In addition, an item asked the patients where they obtained their information about COVID-19 (multiple responses). Finally, the Fear of COVID-19 Scale (hereinafter FC-19s) [15] was included in the questionnaire to assess the respondents’ degree of fear of COVID-19. The section on the FC-19s required the respondents to answer 7 questions using a Likert-type scale ranging from 1 to 5; the higher the overall score was, the higher the respondent’s degree of fear.
Through computerized medical records, the subject’s age, education, and diagnosis were reconfirmed. The patient’s psychopathology was directly determined by a psychiatrist and was measured using the Clinical Global Impressions Scale Severity Score (CGI-S) and the Global Assessment Functioning Scale (GAF).
Descriptive statistics (mean, standard deviation [SD]) were computed for demographic variables. The years of education among the three groups were analyzed by ANOVA, and post hoc analysis (Scheffe) was performed. Student’s t test was performed on each group to compare the differences between the mean values of the CGI-S, GAF, and FC-19. Categorical variables such as sex, changes in daily life, and knowledge about COVID-19 were compared with the χ2 test. The percentage of participants who selected each response was computed. Descriptive statistics were analyzed using SPSS 22 edition for Windows (IBM SPSS Statistics 22; IBM Corp., Armonk, NY, USA). For all statistical analyses, a value of p<0.05 was considered statistically significant.
A total of 278 patients diagnosed with schizophrenia (161 inpatients, 117 outpatients) and 40 nonpatients were recruited. The participants’ gender distributions showed that there were 65 male (40.4%) inpatients, 50 male (42.7%) outpatients, and 13 males (32.5%) in the nonpatient group. There were no significant differences between these groups. The average age was 54.8 years for inpatients, 47.2 years for outpatients, and 46.3 years for the normal control group. The average number of years of education was 10.9 years for the inpatients, 12.8 years for the outpatients, and 15.8 years for the nonpatient group, which indicated a significant difference between the three groups. The average CGI-S score for psychological symptoms was 4.8 for inpatients and 3.6 for outpatients, and the average GAF score was 44.1 points for inpatients and 55.5 points for outpatients. Both evaluation scales showed no significant differences between the two groups (Table 1).
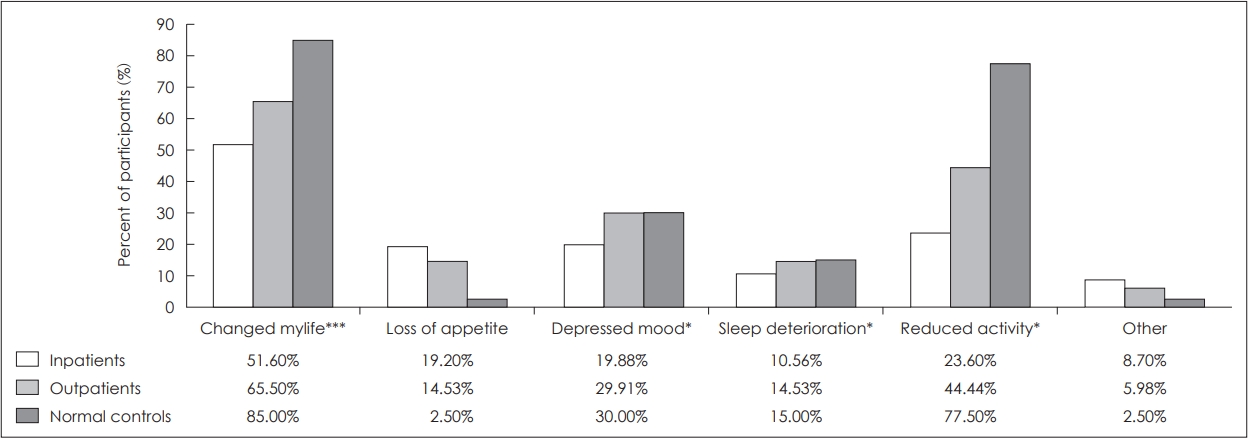
When asked if there had been any change in their lives due to COVID-19, among the inpatients, 51.6% answered positively, followed by 65.5% of the outpatients and 85.0% of the nonpatient respondents (Fig. 1). In the nonpatient group, 77.5% of the respondents reported a decrease in their level of activity, and 30% reported a decrease in their mood. In the schizophrenic patient group, decreased activity levels, decreased mood, decreased appetite, and poor sleep were reported (Fig. 1).
Other responses from patients with schizophrenia reported that among the inpatients, 6 had decreased their walking time, 3 had difficulty going out and staying out, and 6 had difficulty taking walks or going to the store. Others also reported discomfort due to frequent body temperature checks and hand washing and exhibited signs of nervousness and anxiousness. Outpatients complained about the difficulties related to wearing masks, decreased income, and not being able to use saunas and swimming pools.
To date, compared to the 69.2% of the nonpatient respondents who answered that the cumulative number of confirmed COVID-19 cases was between 10,001 and 100,000, only 25.3% of the inpatients and 41.4% of the outpatients were aware of this correct answer (Fig. 2). A total of 15.4% of the nonpatient group, 55.4% of the inpatients and 46.5% of the outpatients answered that the cumulative number of confirmed cases was 10,000 or less. The cumulative number of COVID-19 cases was perceived to be lower in the order of inpatients, outpatients and normal controls (The cumulative number of confirmed patients was 10,001 and 100,000 at the time of the survey).
None of the normal controls thought that the mortality rate would be less than 5%, while 45% of inpatients and 63% of outpatients responded that the mortality rate from COVID-19 was less than 5% (Fig. 3). Seventy-five percent of normal controls, 62% of outpatients and 57% of inpatients responded that the mortality rate of the common cold was less than 1% (Fig. 4). The mortality rates of COVID-19 and the common cold were higher in the order of inpatients, outpatients and normal controls (The mortality rate from COVID-19 in Koreas was less than 5% at the time of the survey).
Regarding the main route of SARS-CoV-2 infection, all of the normal controls except for the nonresponders selected that the disease was transmitted ‘by contaminated saliva,’ whereas various routes of infection were selected by patients with schizophrenia (Fig. 5). The most common option selected by these patients was ‘contaminated saliva’ (inpatient 41.6%, outpatient 82.9%), while other answers consisted of ‘contaminated food’ (inpatient 18.6%, outpatient 9.4%) or ‘mosquito bites’ (inpatient 13.7%). Various other options were also selected (Fig. 5).
Next, for the main symptoms of COVID-19, cough and fever were selected by 95% of normal controls and more than 80% of the outpatients (Fig. 6). In the case of inpatients, symptoms such as cough (74.5%), fever (65.2%), shortness of breath (58.4%), skin rash (29.8%), constipation (25.5%), and dysuria (20.5%) were chosen (Fig. 6).
For preventive measures regarding the transmission of COVID-19, almost all normal controls and outpatients selected items such as ‘wearing a medical mask,’ ’washing hands,’ and ‘avoiding touching your eyes, nose and mouth with unclean hands.’ The answers ‘avoiding people with fever’ and ‘gargling mouthwash’ were also selected at a high rate (Fig. 7). However, the inpatients with schizophrenia were all items, which were ‘wearing a medical mask,’ ‘avoiding touching the eyes, nose and mouth with unclean hands,’ and ‘avoiding people with fever’ and ‘gargling mouthwash,’ also selected other measures such as ‘getting a pneumonia shot,’ ’eating garlic,’ ’taking antibiotics,’ ‘consuming alcohol-based disinfectant,’ and ‘rinsing nasal cavity with saline’ (Fig. 7).
When asked about whether “the most effective way to prevent COVID-19 infection is to wash your hands and wear a mask,” more than 90% of all groups recognized this as the correct answer (Fig. 8). However, 25% of the inpatients and 5% of the outpatients thought that ‘young people cannot get infected with SARS-CoV-2.’ In addition, 46.9% of the inpatients and 11.3% of the outpatients said that ‘there are currently vaccinations and treatments against COVID-19’ (Fig. 8). (There was no vaccine or treatment at the time of the survey.) Approximately 60%-70% of the patients with schizophrenia were aware that ‘the death rate from COVID-19 increases when there is another underlying disease.’ In addition, 56.3% of the inpatients, 27.8% of the outpatients, and 7.7% of the non-patients answered incorrectly to ‘you should use public transportation to go to the hospital if you have a fever or cough after going to church’ (Fig. 8). In addition, 53.8% of the inpatients and 36.5% of the outpatients thought that if they received a letter or package from China, they were more likely to contract COVID-19 (Fig. 8). A total of 31.3% of the inpatients, 15.7% of the outpatients, and 7.7% of the nonpatients answered that it is certain that COVID-19 was deliberately created by and spread from China (Fig. 8).
More than 80% of the patients with schizophrenia responded that their information related to the virus was obtained through TV, while 97.5% of the nonpatient group collected information through the internet (Fig. 9). Other channels of information included radio (56.9%), medical staff (40.0%), and newspapers (23.8%) for inpatients; outpatients reported using the internet (48.8%), family (29.9%), and the radio (27.6%) as their sources of information (Fig. 9).
The average scores on the Fear of COVID-19 Scale were 19.7 points for inpatients, 19.0 points for outpatients, and 16.0 points for nonpatients. Compared to the nonpatient group, inpatients and outpatients had a higher degree of subjective fear of COVID-19 (Table 1).
This study used a questionnaire to investigate the effects of COVID-19 on daily life and whether the current status and knowledge of COVID-19 were properly recognized in 278 patients with schizophrenia and 40 normal control patients.
A total of 85.0% of normal controls answered that the disease had affected their daily life, but only 51.6% of inpatients and 65.5% of outpatients answered this question positively. Unlike the inpatients living in closed wards, approximately 35% of the outpatients reported that there had been no change in their daily life even though they lived at home. Despite the fact that social distancing was becoming a daily routine due to COVID-19, it seems that it had little effect on these respondents because they already tended to stay indoors and were isolated from society.
According to the ‘General Briefing on the Current Status of COVID-19 in Korea’ released by the Central Disease Control Headquarter of the Korea Centers for Disease Control and Prevention, the total cumulative number of COVID-19 confirmed cases in Korea on September 29, 2020, at the time of this survey was 23,699, and the domestic mortality rate at this time was 1.72% [16].
Cognitive errors in the current status of cumulative confirmed cases and mortality of COVID-19 were shown to be higher in the patient group than in the normal group. In patients with schizophrenia, the cumulative status of confirmed COVID-19 patients was underestimated, and the mortality rate was overestimated. The rate of errors was higher in inpatients than in outpatients. This result may be related to a higher score regarding the subjective fear of COVID-19 in the schizophrenic patient group in this study [17]. In addition, the close environment of inpatients and social isolation of outpatients may have affected it.
For the main route of SARS-CoV-2 infection, all the participants in the nonpatient group chose ‘transmission by saliva,’ whereas only 82.9% of outpatients and 41.6% of inpatients chose this answer. However, when asked for ‘the most effective way to prevent COVID-19,’ the answer of washing hands and wearing masks was chosen by more than 90% of all participants. It was found that patients with schizophrenia, especially inpatients, were unable to match the infection route with the appropriate preventive actions. The patients seem to have accepted and remembered a phrase that promoted mask wearing and hand washing observed through media such as TV.
The understanding of COVID-19 symptoms was high in the order of normal patients, outpatients, and inpatients. The main reason for this outcome is the large difference between the external environment of outpatients and the isolated living environment of inpatients, as well as differences in the severity of psychotic symptoms, cognitive ability, education, and length of hospitalization, which may contribute to the outcome disparities; thus, these factors cannot be excluded from the results of this study. They are not exactly aware of the symptoms of COVID-19, so they are less likely to be tested on their own when they show symptoms related to COVID-19 [18].
In this study, 56.3% of the inpatients and 27.8% of the outpatients answered yes to the statement, “If you have a fever or cough after going to church, you should use public transportation to go to the hospital.” According to the Korea Centers for Disease Control and Prevention’s guidelines for preventing the spread of the coronavirus, when one has a suspected symptom of COVID-19, one should avoid going out as much as possible due to concerns of transmission, contact the Centers for Disease Control and Prevention to follow their instructions, and use one’s own transportation to get to a hospital if necessary. However, the results of the current study show that patients with schizophrenia are not aware of the guidelines for initial responses to COVID-19, which increases the risk of further transmission.
In this study, these patients received the most information about COVID-19 through TV and were simply aware of the message, “The most effective way to prevent COVID-19 is to wash your hands and wear a mask.” The results of previous studies have shown that public announcements through clear channels such as television can effectively deliver information about the importance of hand washing and social distancing to schizophrenic patients to help them enact such measures [19]. However, they still have false perceptions of the virus, such as the path of infection, symptoms, and coping measures related to COVID-19.
Guidance to the general public is not sufficient for patients who have schizophrenia due to their limited cognitive abilities. Thus, there is a need for in-hospital education and publicity on specific and direct health and hygiene rules specialized for patients with schizophrenia. Even amidst the COVID-19 pandemic, if such patients are educated simply and well trained, they can participate in infection prevention actions. It is known that patients with schizophrenia generally performed well-known preventive practices, such as hand washing, during the influenza pandemic [20]. Thus, this can be applied not only for the COVID-19 pandemic but also for other infectious diseases in the future. Furthermore, considering that the incidence and mortality rate of COVID-19 in patients with schizophrenia are high [21,22] and that this population is more vulnerable to COVID-19 due to a lack of thorough management of accompanying underlying diseases [8,9], vaccination against COVID-19 needs to be considered first for patients with schizophrenia [23].
Surprisingly, there were remarkably incorrect answers given for several items, even by the nonpatient group. In particular, 40% of the respondents in this group selected “gargling mouthwash” as one of the preventative measures, which was not significantly different from the results of the schizophrenic patient group. A total of 7.7% of normal controls answered ‘yes’ incorrectly to the items ‘COVID-19 was deliberately created by and spread in China’ and ‘If you have a fever or cough after attending church, you should go to the hospital by public transportation’ (Fig. 7). In another study composed of a large-scale sample of the general public, approximately 25% of the respondents said that they went to receive medical services when they experienced symptoms and believed in the conspiracy theory related to China [14]. All of these misunderstandings can be seen in the list of “Breaking Superstitions” on the WHO website [24]. These inaccuracies seem to be due to inaccurate information about COVID-19 being distributed through social media and many other outlets [25].
This study has several limitations. First, the degree of cognitive ability, duration of illness, length of hospitalization, and psychological symptoms of the recruited schizophrenic patient group were not considered when determining the possible effects on their perception of COVID-19. Second, it is difficult to say that the current study represents a larger population of the general public because the nonpatient study group used was very small and consisted only of hospital staff. They will have a higher understanding of diseases than the general public, so the difference in the study results may have been greater. Third, the COVID-19 situation changed between when the participants filled out the questionnaire and when vaccines were developed.
The current study shows that the awareness of COVID-19 among patients with schizophrenia was insufficient, such as the path of infection, symptoms, and coping measures related to COVID-19. In particular, inpatients were not as able to recognize COVID-19 as outpatients. Additional measures are needed to provide information on and accurate statuses regarding COVID-19 to patients with schizophrenia, and priority vaccination needs to be considered for them.
Acknowledgments
This research was supported by research funding from the Yongin Psychiatric Research Institute affiliated with the Yongin Hospital Maintenance Foundation.
Fig. 2.
Answers to the cumulative number of COVID-19 confirmed cases in Korea. Statistics were analyzed by chi-square test. p<0.001.
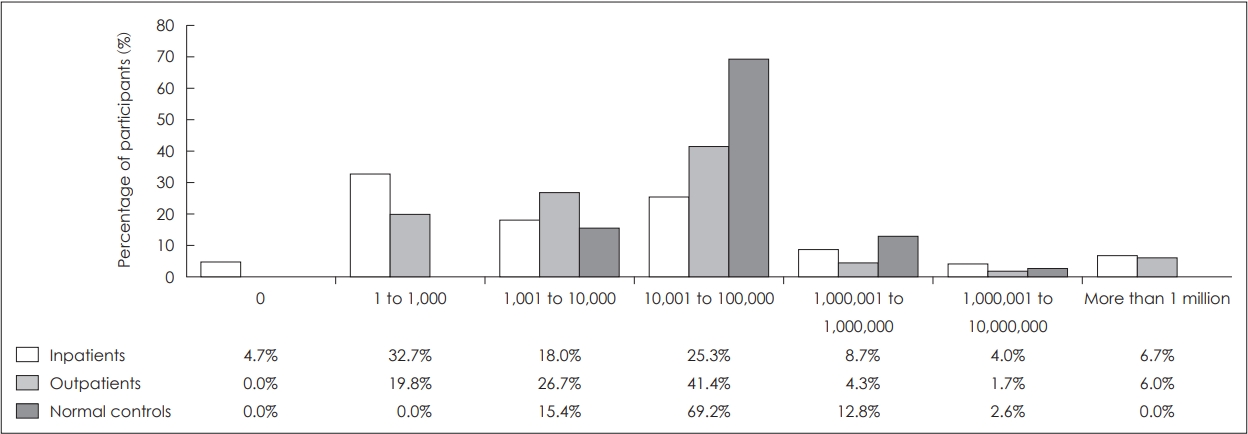
Fig. 3.
Answers to mortality rate of COVID-19 in Korea. Statistics were analyzed by chi-square test. p<0.001.
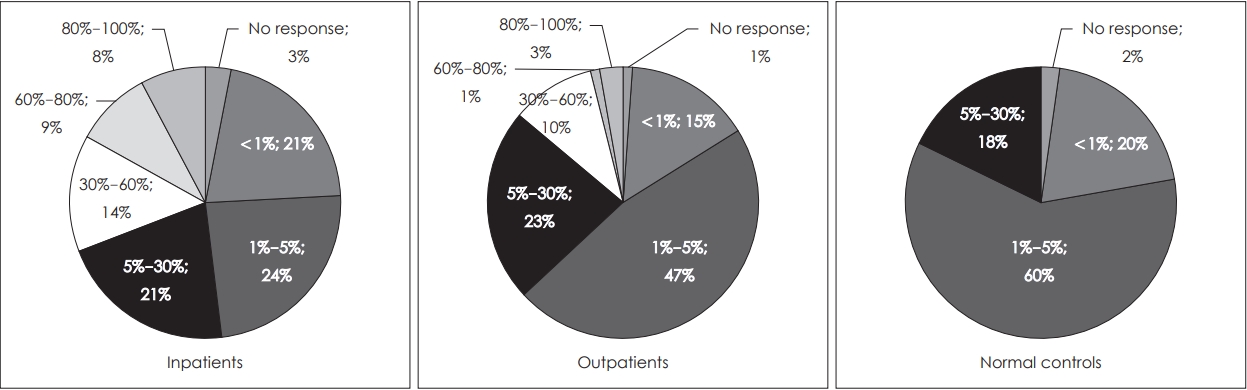
Fig. 4.
Answers to mortality from a common cold. Statistics were analyzed by chi-square test. p<0.05.
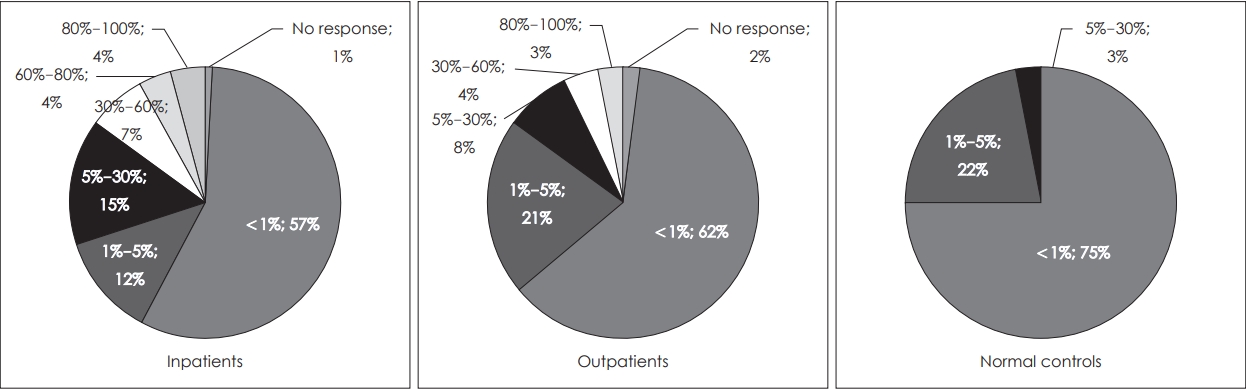
Fig. 5.
Proportion of the main transmission route of COVID-19 selected by participants. Statistics were analyzed by chi-square test. p<0.001.
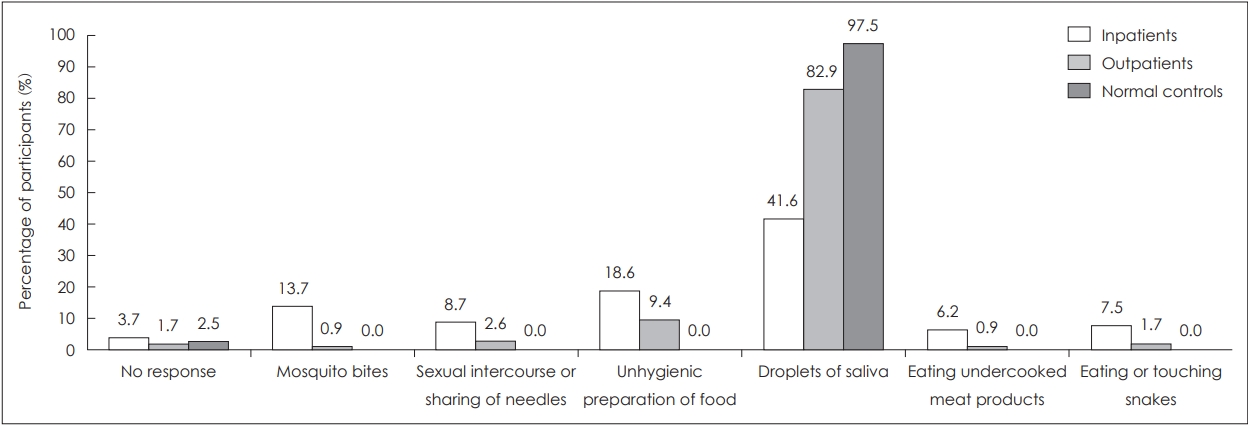
Fig. 6.
Proportion of participants who replied “yes” to each item to identify the main symptoms of COVID-19 infection (multiple responses). Statistics were analyzed by chi-square test. *p<0.05; ***p<0.001.
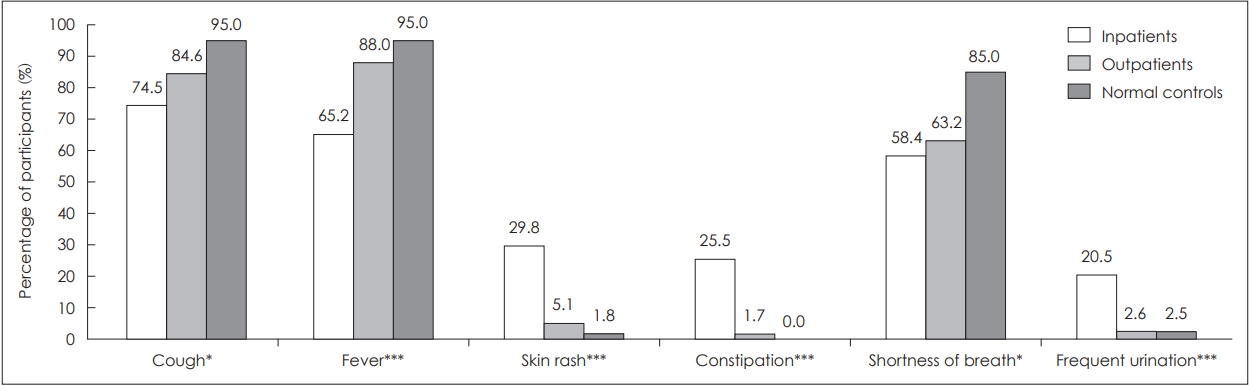
Fig. 7.
Proportion of participants who replied “yes” to each item to identify whether each of these 10 actions act as prevention measures against COVID-19 infection (multiple responses). Statistics were analyzed by chi-square test. *p<0.05; ***p<0.001.
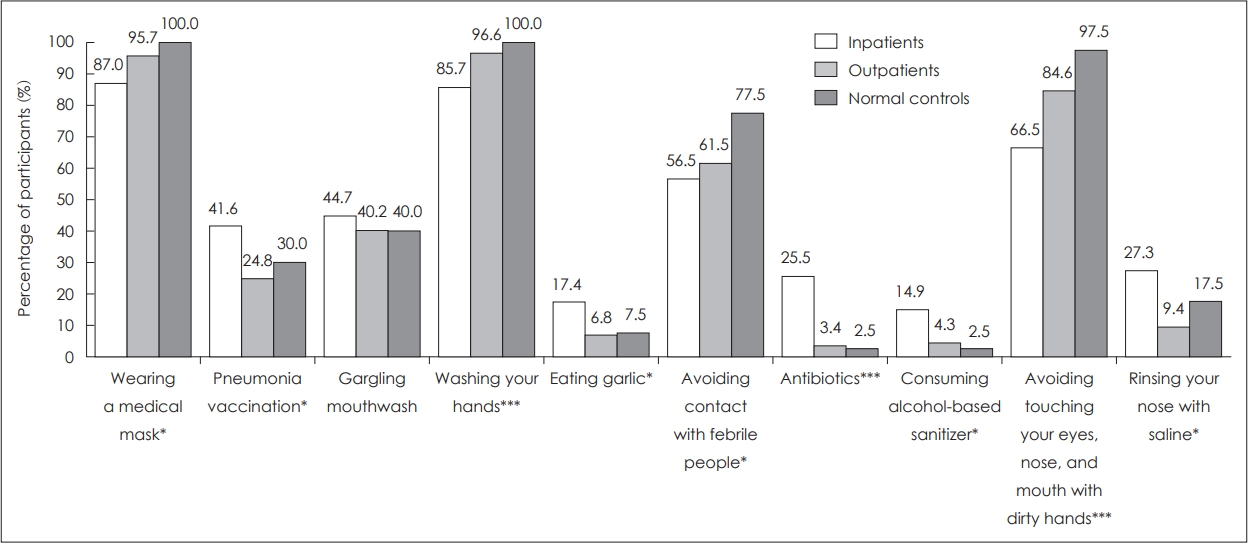
Fig. 8.
Proportion of participants who replied “yes” toeach item to identify misperceptions about COVID-19. Statistics were analyzed by
chi-square test. *p<0.05; ***p<0.001.
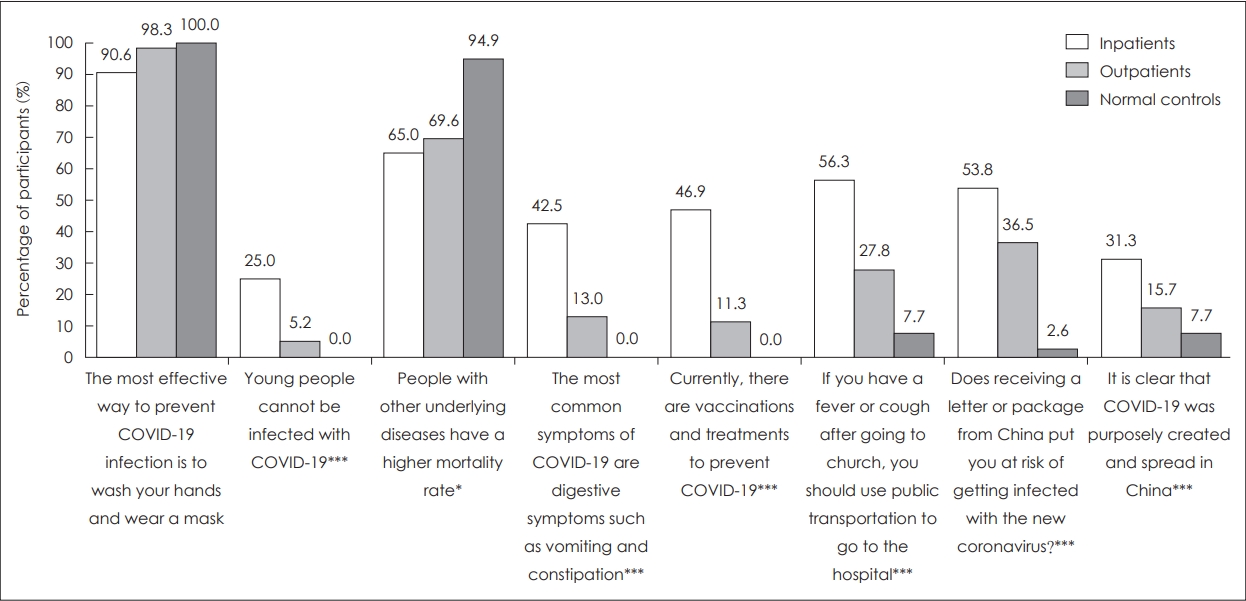
Fig. 9.
Proportion of participants who replied “yes” toeach item to identify ways to obtain information about COVID-19 (multiple
responses). Statistics were analyzed by chi-square test. *p<0.05; ***p<0.001.
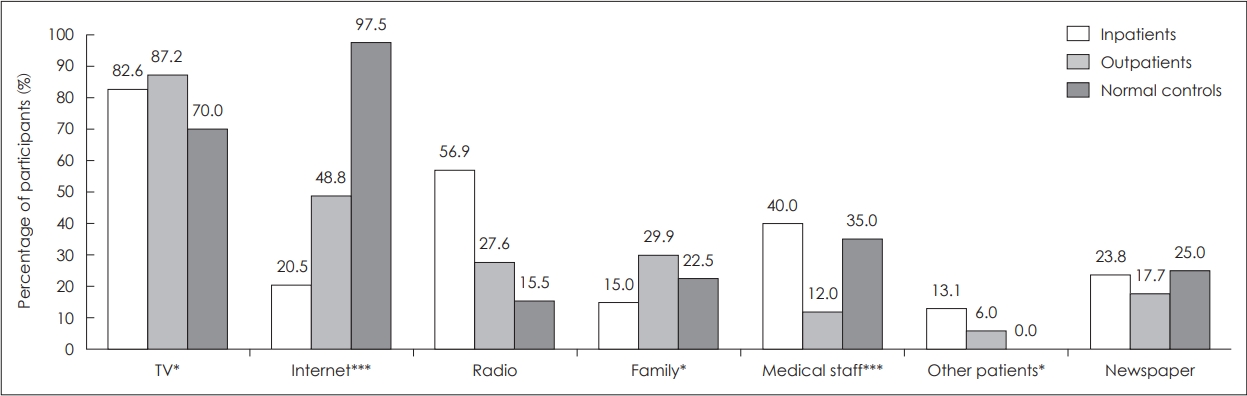
Table 1.
Demographic characteristics and the fear of COVID-19 scale among inpatients, outpatients with schizophrenia and normal (n=318)
| Inpatients with SPR (n=161) | Outpatients with SPR (n=117) | Normal (n=40) | p-value | Scheffe* | |
|---|---|---|---|---|---|
| Age (years) | 54.8±10.8 | 47.2±12.0 | 46.3±15.3 | <0.01 | a>b, c |
| Educational year | 10.9±3.8 | 12.8±2.8 | 15.8±3.1 | <0.01 | a<b<c |
| Sex (male) | 65 (40.4) | 50 (42.7) | 13 (32.5) | 0.52 | |
| CGI-S | 4.8±1.0 | 3.6±1.2 | 0.37 | ||
| GAF | 44.1±11.7 | 55.5±13.6 | 0.32 | ||
| FC-19s | 19.7±6.0 | 19.0±5.5 | 16.0±4.7 | <0.01 | a, b>c |
REFERENCES
1) WHO. WHO Coronavirus Disease (COVID-19) Dashboard 2022 Sep 14; Available from: https://covid19.who.int/.
2) Jeon HL, Kwon JS, Park SH, Shin JY. Association of mental disorders with SARS-CoV-2 infection and severe health outcomes: nationwide cohort study. The British Journal of Psychiatry 2021;218:344-351.


3) Wang Q, Xu R, Volkow ND. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry 2021;20:124-130.




4) Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry 2020;7:e21.



5) Larkin A, Hutton P. Systematic review and meta-analysis of factors that help or hinder treatment decision-making capacity in psychosis. The British Journal of Psychiatry 2017;211:205-215.


6) Maguire PA, Reay RE, Looi JC. Nothing to sneeze at-uptake of protective measures against an influenza pandemic by people with schizophrenia: willingness and perceived barriers. Australasian Psychiatry 2019;27:171-178.




7) Van Haaster I, Lesage A, Cyr M, Toupin J. Problems and needs for care of patients suffering from severe mental illness. Social psychiatry and psychiatric epidemiology 1994;29:141-148.



8) Fonseca L, Diniz E, Mendonca G, Malinowski F, Mari J, Gadelha A. Schizophrenia and COVID-19: risks and recommendations. Brazilian Journal of Psychiatry 2020;42:236-238.



9) Kozloff N, Mulsant BH, Stergiopoulos V, Voineskos AN. The COVID-19 Global Pandemic: Implications for People With Schizophrenia and Related Disorders. Schizophr Bull 2020;46:752-757.




10) Shinn AK, Viron M. Perspectives on the COVID-19 pandemic and individuals with serious mental illness. The Journal of Clinical Psychiatry 2020;81:14205.

11) Bradford DW, Kim MM, Braxton LE, Marx CE, Butterfield M, Elbogen EB. Access to medical care among persons with psychotic and major affective disorders. Psychiatric Services 2008;59:847-852.


12) Muruganandam P, Neelamegam S, Menon V, Alexander J, Chaturvedi SK. COVID-19 and severe mental illness: impact on patients and its relation with their awareness about COVID-19. Psychiatry research 2020;291:113265.



13) Thomson S, Doan T, Liu D, Schubert KO, Toh J, Boyd MA, et al. Supporting the vulnerable: developing a strategic community mental health response to the COVID-19 pandemic. Australas Psychiatry 2020;1039856220944701.


14) Geldsetzer P. Use of rapid online surveys to assess people’s perceptions during infectious disease outbreaks: a cross-sectional survey on COVID-19. J Med Internet Res 2020;22:e18790.



15) Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict 2022;20:1537-1545.




16) Coronavirus Infectious Disease-19 Outbreak in Korea. 2020 Sep 29; Available from: http://ncov.mohw.go.kr/tcmBoardView.do?brdId=&brdGubun=&dataGubun=&ncvContSeq=360121&contSeq=360121&board_id=140&gubun=BDJ.
17) Natale A, Concerto C, Rodolico A, Birgillito A, Bonelli M, Martinez M, et al. Risk perception among psychiatric patients during the COVID-19 pandemic. Int J Environ Res Public Health 2022;19:2620.



18) Teixeira AL, Krause TM, Ghosh L, Shahani L, Machado-Vieira R, Lane SD, et al. Analysis of COVID-19 infection and mortality among patients with psychiatric disorders, 2020. JAMA Netw Open 2021;4:e2134969.



19) Maguire PA, Looi JC. Vulnerability of people with schizophrenia to COVID-19. Aust N Z J Psychiatry 2020;54:1044.



20) Maguire PA, Reay RE, Looi JCL. Nothing to sneeze at-uptake of protective measures against an influenza pandemic by people with schizophrenia: willingness and perceived barriers. Australasian Psychiatry 2018;27:171-178.




21) Tzur Bitan D, Krieger I, Kridin K, Komantscher D, Scheinman Y, Weinstein O, et al. COVID-19 prevalence and mortality among schizophrenia patients: a large-scale retrospective cohort study. Schizophrenia Bulletin 2021;47:1211-1217.




22) Fond G, Nemani K, Etchecopar-Etchart D, Loundou A, Goff DC, Lee SW, et al. Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: a systematic review and meta-analysis. JAMA psychiatry 2021;78:1208-1217.



23) De Hert M, Mazereel V, Detraux J, Van Assche K. Prioritizing COVID-19 vaccination for people with severe mental illness. World Psychiatry 2021;20:54.




24) WHO. Coronavirus disease (COVID-19) advice for the public: Myth busters. 2020 Sep 29; Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters.
25) Romm T. Millions of tweets peddled conspiracy theories about coronavirus in other countries, an unpublished U.S. report says. 2020; Available from: https://www.washingtonpost.com/technology/2020/02/29/.
-
METRICS

-
- 0 Crossref
- Scopus
- 1,203 View
- 12 Download
- Related articles in Korean J Schizophr Res
-
Effects of Token Economy Intervention on Hospitalized Patients With Schizophrenia2023 April;26(1)
Correlates of Violence in Patients with Schizophrenia.2015 April;18(1)
Characteristics of Ambivalence of Self-image in Patients with Schizophrenia.2016 April;19(1)